Guest Author: Seth Kaplan
Many people take calcium without knowing why. When I ask them if a healthcare professional told them to take it, they often reply, “Nope. I just take it,” or “It’s good for bones and preventing osteoporosis, so I take it.” While the second of these answers is true, there is a lot more information for you and your doctor to assess before deciding whether to supplement with calcium.
What is calcium and why do you need it?
Calcium is a mineral that is essential for life. Calcium builds bones and keeps them healthy, helps blood to clot, nerves to send messages, and muscles to contract . Once calcium is absorbed—and absorption is the key concept because minerals compete for absorption—the blood carries it to the cells and through cell membranes in a form the cells can use. About 99 % of the calcium in our bodies is in our bones and teeth.
 The body also loses calcium every day by shedding hair, skin, and nails and through sweat, urine, and feces. Lost calcium must be replaced.
The body also loses calcium every day by shedding hair, skin, and nails and through sweat, urine, and feces. Lost calcium must be replaced.
When you talk about nutrition with your friends, you will find that they take different kinds of calcium in differing amounts. Especially with calcium, knowing how much to take and which form offers the greatest benefit are important. Here are guidelines you can review with your doctor:
- 19 to 50 years: 1,000 mg/day
- 51 to 70 years: Men – 1,000 mg/day;
- 51 to 70 years: Women – 1,200 mg/day
- 71 years and over: 1,200 mg/day
Different Forms
Read the labels and you will find that calcium supplements employ several different forms of calcium. Each compound contains varying amounts of the mineral calcium — referred to as elemental calcium. Common calcium supplements may be labeled as:
- Calcium carbonate (40 percent elemental calcium) – the cheapest form; used the most often.
- Calcium citrate (21 percent elemental calcium) – the best-absorbed form.
- Calcium gluconate (9 percent elemental calcium)
- Calcium lactate (13 percent elemental calcium)
Note: Do not use antacids like Tums as a source of supplemental calcium. Antacids can also contain sodium, aluminum, and sugar, which can have negative interactions with calcium.
What helps with calcium absorption?
When you read the labels on bottles of calcium supplements, you will often see other ingredients included. The two most common are Vitamin D3 and magnesium. Both of these help with absorbing the maximum amount of calcium from both foods and supplements. Once you have absorbed all that calcium, however, how can you be sure that it will arrive at the parts of the body that use it most — the teeth and bones? The answer to this question is an interesting scientific anecdote, and should be a topic of discussion with your doctor when discussing calcium supplementation.
Vitamin K2
 About 10 years ago, epidemiologists stumbled upon a nutritional contradiction: In developed countries like the United States, where all the calcium you could ever want is available, the number of knee and hip replacements and other bone-related maladies was rising rapidly. Yet, in undeveloped countries, where calcium was hard to get because of poor diets or low incomes, very few joint replacements were performed. How could this paradox exist?
About 10 years ago, epidemiologists stumbled upon a nutritional contradiction: In developed countries like the United States, where all the calcium you could ever want is available, the number of knee and hip replacements and other bone-related maladies was rising rapidly. Yet, in undeveloped countries, where calcium was hard to get because of poor diets or low incomes, very few joint replacements were performed. How could this paradox exist?
Epidemiologists and biochemists got to work and, after numerous studies, an answer emerged: Vitamin K2, a.k.a. menaquinone. High dietary intake of vitamin K2 influences cardiovascular health and reduces cardiovascular mortality. More specifically, as it relates to calcium, Vitamin K2 prevents some of the total absorbed calcium from adhering to heart blood vessels, which is called calcification. Today, about 60% of Americans have calcification.
Potential problems when taking calcium
Because 500 millligrams is the most calcium that the body can absorb in one dose, most recommendations suggest splitting the calcium dose throughout the day; e.g., to get 1000 milligrams, take 500 milligrams in the morning and 500 milligrams in the evening. Other potential interactions that can occur:
- Corticosteroids: If you are on corticosteroid therapy for longer than six weeks, take an extra 300-500 milligrams of calcium.
- Sodium: Sodium increases the amount of calcium excreted in the urine, so take more calcium if you eat foods high in salt.
- Excess protein: The body uses excess protein for energy. However, as protein is burned for energy, it produces sulfate. Sulfate increases the amount of calcium excreted in the urine, which decreases the amount of calcium in the body. Excess protein creates excess sulfate.
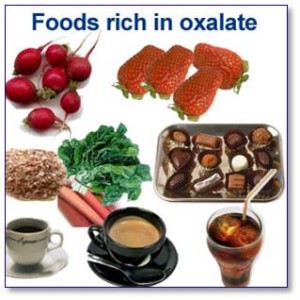 Oxalate: Found in spinach, chard, berries, chocolate, and tea, oxalate binds with calcium and increases the loss of calcium through bowel movements. For example, even though sweet potatoes contain calcium, not all of it is absorbed because of the oxalic acid (oxalate) they contain.
Oxalate: Found in spinach, chard, berries, chocolate, and tea, oxalate binds with calcium and increases the loss of calcium through bowel movements. For example, even though sweet potatoes contain calcium, not all of it is absorbed because of the oxalic acid (oxalate) they contain.- Phosphorous: Also known as phosphoric acid and phosphate, phosphorous — which is in cola and many processed foods — can interfere with calcium absorption.
- Insoluble fiber: This type of fiber, such as the kind in wheat bran, reduces calcium absorption.
- Alcohol intake: Drinking excessive amounts of alcohol can interfere with the calcium balance by inhibiting the enzymes that convert inactive vitamin D to active vitamin D.
- Caffeine: Excessive intake of caffeine (300 mg-400 mg) can increase urinary excretion as well as fecal excretion. (One cup [8 fl oz] of brewed coffee contains about 80 mg of caffeine.)
- Smoking, stress, and lack of exercise: These lifestyle factors contribute to the body not being able to absorb calcium as efficiently.
What to take away from this post
The headline is: Do not supplement with calcium casually. Talk to your doctor first. Remember to ask about maximum absorption and calcification. Talk to h/her about how your other medications and supplements might affect supplemental calcium. Then, you can proceed with confidence.
